Years of U.S.-led investment in AIDS programs have significantly lowered AIDS-related deaths to their lowest point in over 30 years and provided critical medications for some of the world’s most vulnerable populations. However, in the past six months, a sudden halt in U.S. funding has caused a severe disruption, with U.N. officials warning that without replacement funding, more than 4 million AIDS-related deaths and 6 million new HIV infections could occur by 2029.
A recent UNAIDS report highlighted how this funding cut has destabilized supply chains, forced health facility closures, left many clinics understaffed, disrupted prevention efforts, slowed HIV testing, and forced community groups to reduce or stop their activities. The report also raised concerns that other major donors might reduce their contributions, threatening decades of global progress against AIDS amid geopolitical tensions, wars, and climate change challenges.
The $4 billion U.S. pledge for HIV programs in 2025 vanished almost overnight in January when President Donald Trump ordered a suspension of all foreign aid and later moved to close the U.S. Agency for International Development (USAID). Andrew Hill, an HIV expert at the University of Liverpool, noted that while the U.S. government can decide how to allocate funds, it was irresponsible to cut funding abruptly without warning, leaving African patients stranded when clinics shut down overnight.
The U.S. President’s Emergency Plan for AIDS Relief (PEPFAR), launched in 2003 under President George W. Bush, is the largest commitment by any nation targeting a single disease. UNAIDS described it as a “lifeline” for countries with high HIV rates, supporting testing for over 84 million people and treatment for more than 20 million. In Nigeria, PEPFAR funded nearly all of the country’s HIV prevention medication budget.
In 2024, approximately 630,000 people died from AIDS globally, a number that has stabilized since 2022 after peaking at around 2 million in 2004. Even before the funding cuts, progress was uneven, with half of all new HIV infections occurring in sub-Saharan Africa.
Tom Ellman, director of Doctors Without Borders’ South Africa Medical Unit, said that while some low-income countries are trying to fund more of their own HIV programs, they cannot replace the scale of U.S. support. He emphasized that nothing can fully protect these countries from the sudden and severe withdrawal of American aid.
Experts also warn of a critical loss in data collection and surveillance, as the U.S. funded much of the HIV monitoring infrastructure in African nations, including hospital records and electronic patient tracking systems. Dr. Chris Beyrer, director of the Global Health Institute at Duke University, stressed that without reliable data on HIV transmission, controlling the epidemic will be extremely difficult.
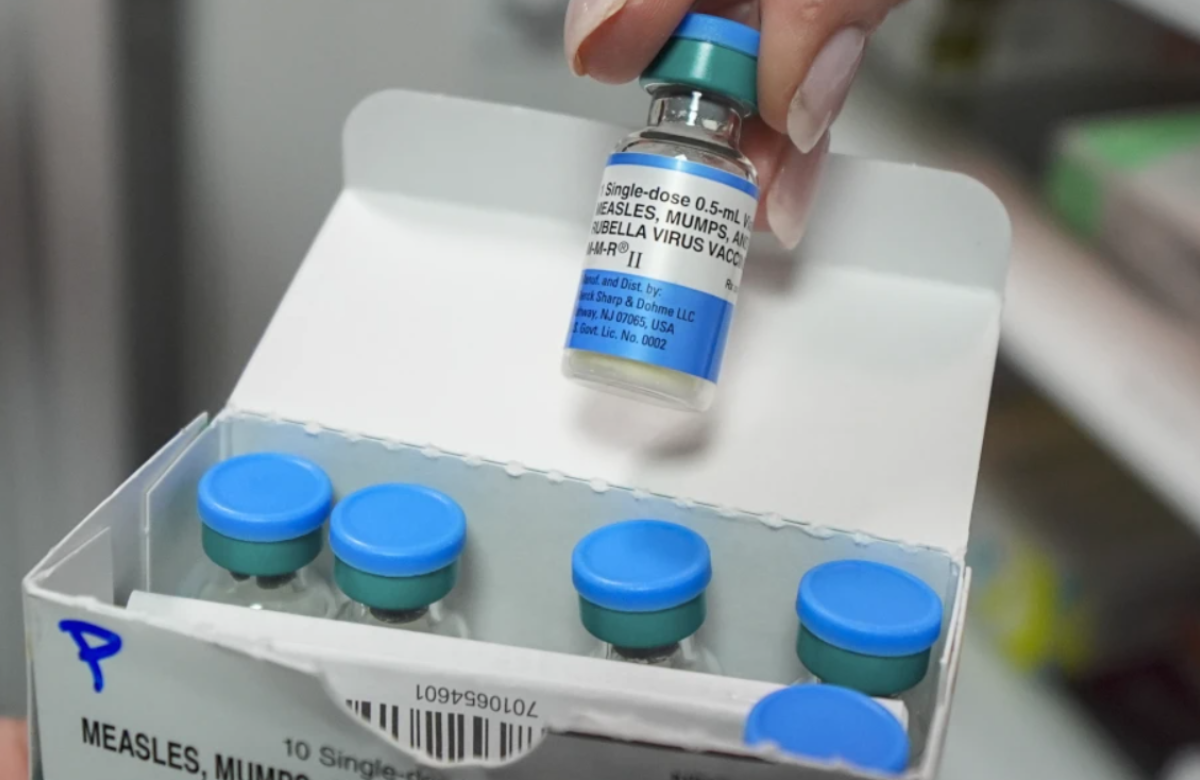
This uncertainty comes at a pivotal time when a twice-yearly injectable drug, developed by pharmaceutical company Gilead, has shown 100% effectiveness in preventing HIV in recent studies. South Africa’s health minister, Aaron Motsoaledi, vowed to ensure every adolescent girl in need receives the drug, acknowledging the continent’s troubling dependence on U.S. aid.
Last month, the U.S. Food and Drug Administration approved the drug, called Yeztugo, a milestone that advocates hoped would mark a turning point in ending AIDS. However, critics like Peter Maybarduk of the advocacy group Public Citizen argue that Gilead’s pricing makes it unaffordable for many countries most affected by HIV. While Gilead has agreed to allow generic versions in 120 poor countries with high HIV rates, nearly all of Latin America—where HIV rates are rising—has been excluded.
Maybarduk concluded, “We could be ending AIDS. Instead, the U.S. is stepping away from the fight.”